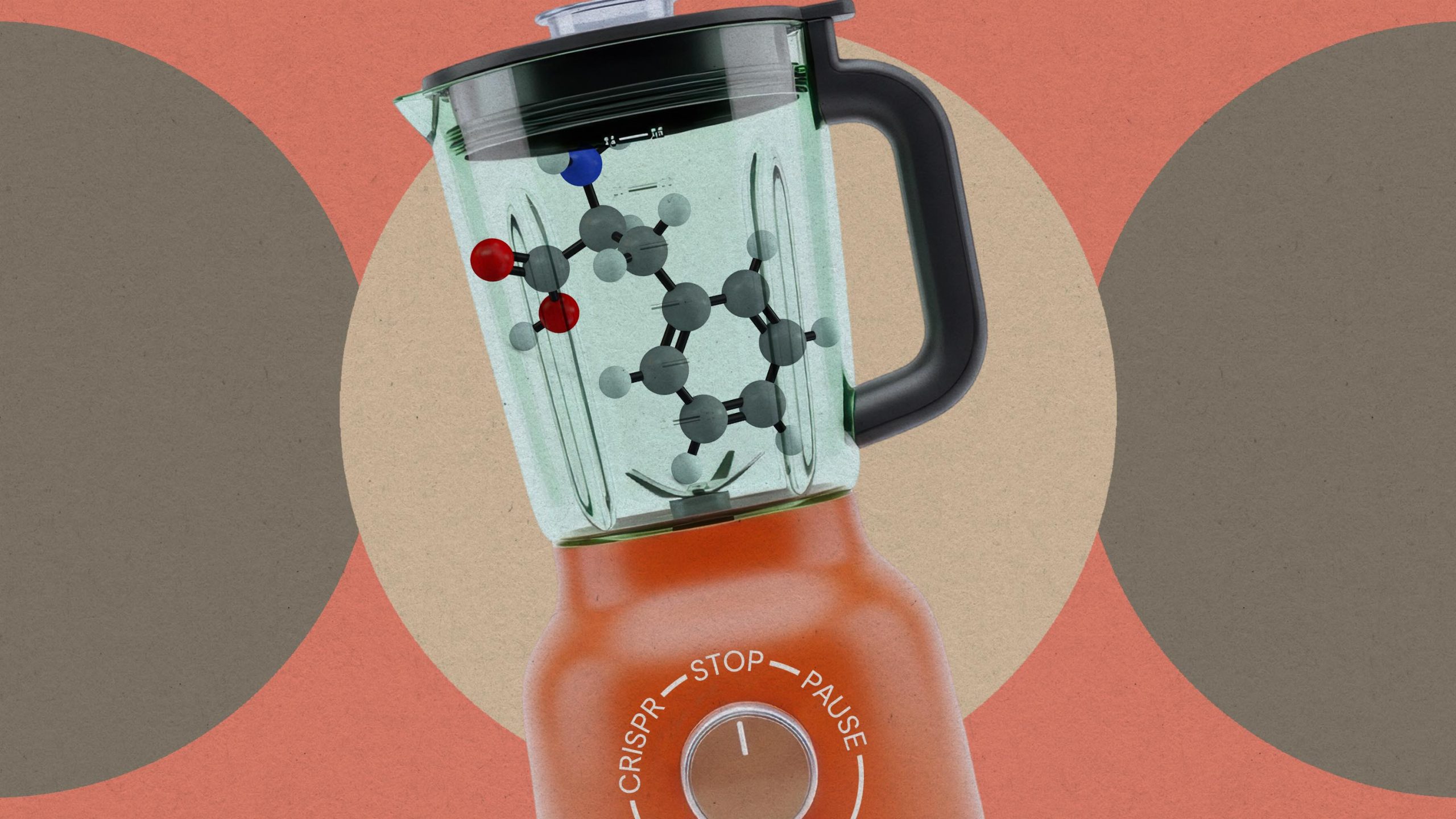
The groundbreaking success of GLP-1 receptor agonist drugs like Ozempic, Wegovy, and Mounjaro in the battle against obesity is increasingly overshadowed by a stark reality: for many users, the journey to sustained weight loss may necessitate a lifelong commitment to these injectables, as discontinuing them often triggers a relentless return of hunger and subsequent weight regain.
These medications, which mimic the natural hormone Glucagon-Like Peptide-1 (GLP-1), have revolutionized weight management by working on multiple fronts: they slow gastric emptying, increase feelings of fullness (satiety), and signal to the brain that the body is nourished, thereby reducing appetite and cravings. For individuals who have struggled for years with traditional diets and exercise, these drugs offer an unprecedented sense of control over their food intake. Tanya Hall, a Wegovy user who shed 83 pounds, eloquently captured this sentiment for the BBC, stating, "For the first 38 years of my life, I was overweight — now I’m six stone (38kg) [83 pounds] lighter. Therefore, there’s part of me that feels like there’s an addiction to keep it going because it makes me feel the way that I feel, it makes me feel in control.” This feeling of newfound agency is powerful, yet it hints at a potential psychological and physiological dependency that extends beyond typical medication adherence.
The scientific literature and anecdotal reports confirm that this perceived "addiction" to control is rooted in physiological changes. Research, including studies conducted by Novo Nordisk, the maker of Ozempic and Wegovy, consistently demonstrates that patients who cease using these medications tend to regain a significant portion—often two-thirds or more—of the weight they initially lost. Physician Hussain Al-Zubaidi corroborated this, noting that he has observed patients regaining 60 to 80 percent of their lost weight. This phenomenon underscores a crucial understanding of obesity: it is not merely a failure of willpower but a complex chronic disease influenced by genetics, environment, and metabolic factors that powerfully resist weight loss and promote regain.
When a person loses weight, the body’s intricate homeostatic mechanisms kick into overdrive to restore its perceived "set point." This involves a cascade of hormonal adjustments designed to encourage eating and conserve energy. Levels of hunger-promoting hormones like ghrelin increase, while satiety hormones like leptin decrease. Simultaneously, the basal metabolic rate, the number of calories the body burns at rest, often slows down, making it even harder to maintain the new, lower weight. GLP-1 agonists effectively counteract these biological forces, but once the medication is stopped, these powerful compensatory mechanisms resurface, often with a vengeance, leaving individuals battling intense cravings and a metabolism geared towards weight regain. This physiological rebound explains why the hunger "comes roaring back," feeling uncontrollable and overwhelming to those who have experienced the suppression provided by the drugs.
This emerging reality has profound implications for how obesity is viewed and treated. Celebrities like Oprah Winfrey, who has openly discussed her use of GLP-1s, articulate this shift by stating her intention to remain on the medication indefinitely. In an interview with People Magazine, she drew a direct parallel to managing other chronic conditions: “It’s going to be a lifetime thing. I’m on high blood pressure medication, and if I go off the high blood pressure medication, my blood pressure is going to go up. The same thing is true now, I realize, with these medications. I’ve proven to myself I need it.” This perspective aligns with a growing consensus in the medical community that obesity should be treated as a chronic condition, much like hypertension, diabetes, or asthma, requiring continuous management rather than a temporary fix.
However, the prospect of lifelong medication raises significant questions regarding accessibility, cost, and long-term health implications. GLP-1 drugs are expensive, and consistent access remains a major barrier for many, especially in healthcare systems where insurance coverage for obesity treatments is often limited or non-existent. The financial burden on individuals and healthcare systems could be astronomical if millions require these drugs for decades. Furthermore, while generally well-tolerated, these medications are not without side effects, which can range from common gastrointestinal issues like nausea, vomiting, diarrhea, and constipation to rarer, more serious concerns such as pancreatitis, gallbladder problems, and a potential risk of thyroid C-cell tumors (though this has primarily been observed in rodent studies). The long-term impact of continuous use on the body’s systems is still being studied, adding another layer of complexity to the "lifelong" commitment.
Another critical concern is the composition of weight lost. While GLP-1s are highly effective at reducing overall body weight, a significant portion of this loss can be lean muscle mass alongside fat. Muscle is metabolically active tissue, meaning it burns more calories at rest than fat. Losing muscle can further depress the metabolic rate, making weight maintenance even more challenging. This emphasizes the crucial role of resistance training and adequate protein intake alongside medication to preserve muscle mass and optimize metabolic health.
Despite these formidable challenges, the narrative is not entirely bleak. Experts like Dr. Al-Zubaidi emphasize the importance of an "exit strategy" for patients hoping to discontinue the drugs without regaining all the lost weight. This strategy centers on leveraging the period of appetite suppression to establish deeply ingrained, healthier lifestyle habits. The drugs provide a window of opportunity where individuals can learn to make better food choices without constant hunger, develop consistent exercise routines, and address psychological triggers for eating.
Ellen Ogley’s experience, also shared with the BBC, serves as a testament to the potential success of such an approach. After losing 48.5 pounds on Eli Lilly’s GLP-1 drug Mounjaro, she focused intensely on incorporating regular exercise and healthier eating patterns into her daily life. Crucially, she sustained these changes even after discontinuing the medication. Her ability to maintain her weight loss demonstrates that while the drugs offer powerful pharmacological support, they are most effective when integrated into a holistic, behavioral change program. "I want people to know that life after Mounjaro can be sustainable as well," she affirmed.
An effective "exit strategy" involves several key components:
- Structured Nutritional Guidance: Working with registered dietitians to develop personalized, sustainable eating plans that focus on nutrient-dense foods, portion control, and mindful eating practices.
- Comprehensive Exercise Regimen: Integrating both cardiovascular exercise for heart health and strength training to preserve and build muscle mass, counteracting the muscle loss often associated with rapid weight reduction.
- Behavioral Therapy: Addressing emotional eating patterns, stress management techniques, and developing non-food-related coping mechanisms. Cognitive Behavioral Therapy (CBT) and other psychological interventions can be invaluable in recalibrating one’s relationship with food.
- Gradual Tapering: While not always feasible or recommended, some clinicians explore gradual dose reduction to allow the body to slowly adapt rather than facing an abrupt cessation of the drug’s effects.
- Ongoing Support: Continued engagement with healthcare providers, support groups, or wellness programs to maintain accountability and address potential setbacks.
Looking ahead, the landscape of obesity treatment continues to evolve rapidly. Next-generation drugs, such as multi-agonists that target not only GLP-1 but also other pathways like GIP (glucose-dependent insulinotropic polypeptide) and glucagon (e.g., tirzepatide, retatrutide), are showing even greater efficacy in weight loss. These compounds may offer different mechanisms of action or potentially a more sustained impact, though the question of long-term dependency will likely persist. Research into personalized medicine, tailoring drug choices and dosages based on individual genetic profiles and metabolic responses, could also optimize outcomes and potentially reduce the need for indefinite use for some.
In conclusion, GLP-1 receptor agonists represent a monumental leap forward in treating obesity, offering a powerful tool that addresses the underlying biology of weight regulation. However, the emerging reality of significant weight regain upon discontinuation highlights that these drugs are not a "cure" but rather highly effective management tools for a chronic disease. For many, they will likely become a lifelong commitment, akin to medication for hypertension or diabetes. For those hoping to transition off these injectables, a robust, medically supervised "exit strategy" that prioritizes profound and sustained lifestyle changes is not merely advisable but essential for achieving lasting weight management. The conversation around GLP-1s must therefore shift from short-term weight loss to comprehensive, long-term health management, acknowledging both their revolutionary potential and their complex implications for individuals and healthcare systems worldwide.