The core of this technological marvel lies in its remarkable duality: an exceptionally small physical footprint coupled with an extraordinary capacity for high-speed data transmission. At its heart is the Biological Interface System to Cortex (BISC), a brain-computer interface (BCI) ingeniously engineered around a single, ultra-thin silicon chip. This chip establishes a wireless, high-bandwidth conduit, seamlessly bridging the intricate network of the brain with external computing systems. The BISC system, detailed in a seminal study published on December 8th in Nature Electronics, comprises three key components: the chip-based implant itself, a wearable "relay station," and the sophisticated software architecture required to operate the entire platform.
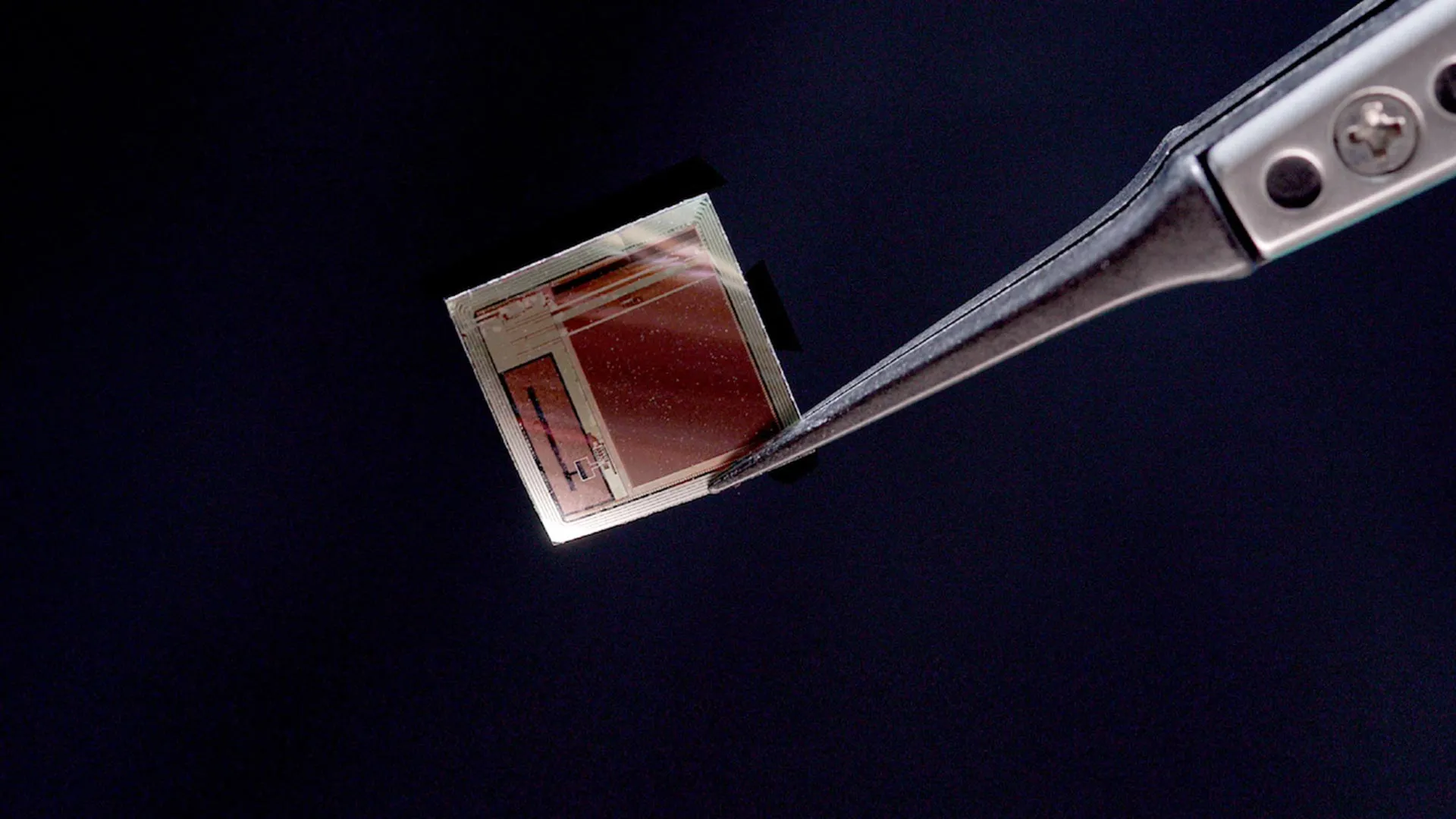
Ken Shepard, the Lau Family Professor of Electrical Engineering, professor of biomedical engineering, and professor of neurological sciences at Columbia University, who spearheaded the engineering efforts as one of the senior authors, highlighted the transformative nature of the implant’s design. "Most implantable systems are built around a canister of electronics that occupies enormous volumes of space inside the body," Shepard explained. "Our implant is a single integrated circuit chip that is so thin that it can slide into the space between the brain and the skull, resting on the brain like a piece of wet tissue paper." This radical departure from traditional bulky implants significantly reduces surgical invasiveness and the potential for tissue disruption.
Collaborating closely with Shepard was Andreas S. Tolias, PhD, a senior and co-corresponding author, professor at the Byers Eye Institute at Stanford University, and co-founding director of the Enigma Project. Tolias’s profound expertise in training artificial intelligence (AI) systems on expansive neural recordings, including those generated by BISC, proved instrumental in assessing the implant’s decoding capabilities. "BISC turns the cortical surface into an effective portal, delivering high-bandwidth, minimally invasive read-write communication with AI and external devices," Tolias stated. "Its single-chip scalability paves the way for adaptive neuroprosthetics and brain-AI interfaces to treat many neuropsychiatric disorders, such as epilepsy." This underscores BISC’s potential to act as a direct interface, enabling AI to understand and interact with brain activity at an unprecedented level.
The clinical dimension of this pioneering work was championed by Dr. Brett Youngerman, assistant professor of neurological surgery at Columbia University and a neurosurgeon at NewYork-Presbyterian/Columbia University Irving Medical Center, who served as the project’s principal clinical collaborator. "This high-resolution, high-data-throughput device has the potential to revolutionize the management of neurological conditions from epilepsy to paralysis," Dr. Youngerman asserted. His collaboration, alongside Shepard and Dr. Catherine Schevon, an epilepsy neurologist at NewYork-Presbyterian/Columbia, has already yielded significant progress, including securing a National Institutes of Health grant to investigate BISC’s application in treating drug-resistant epilepsy. Dr. Youngerman emphasized the core tenets of effective BCI development: "The key to effective brain-computer interface devices is to maximize the information flow to and from the brain, while making the device as minimally invasive in its surgical implantation as possible. BISC surpasses previous technology on both fronts." This dual focus on maximizing data exchange while minimizing physical intrusion represents a significant leap forward.
Shepard further elaborated on the impact of modern semiconductor technology, drawing a parallel between the evolution of personal computing and medical implants. "Semiconductor technology has made this possible, allowing the computing power of room-sized computers to now fit in your pocket," he remarked. "We are now doing the same for medical implantables, allowing complex electronics to exist in the body while taking up almost no space." This analogy effectively conveys the miniaturization and power enhancement achieved with BISC.
The engineering behind BISC represents a paradigm shift in BCI design. Traditional medical-grade BCIs typically necessitate multiple discrete microelectronic components, such as amplifiers, data converters, and radio transmitters. These components are conventionally housed within a relatively substantial implanted canister, often requiring invasive skull removal or placement elsewhere in the body, with wires extending to the brain. BISC, in stark contrast, integrates the entire system onto a single complementary metal-oxide-semiconductor (CMOS) integrated circuit. This chip has been meticulously thinned to a mere 50 micrometers, occupying less than one-thousandth of the volume of a conventional implant. With an overall size of approximately 3 cubic millimeters, this flexible chip can conform to the contours of the brain’s surface. This micro-electrocorticography (µECoG) device is astonishingly dense, boasting 65,536 electrodes, 1,024 recording channels, and a remarkable 16,384 stimulation channels. Crucially, the chip’s production utilizing established semiconductor industry manufacturing methods ensures its suitability for large-scale, cost-effective production.
The integrated nature of the BISC chip is a key innovation. It seamlessly incorporates a radio transceiver, a wireless power circuit, digital control electronics, power management systems, data converters, and the essential analog components for both recording and stimulation. The external relay station serves as the crucial link, providing both power and data communication through a custom ultrawideband radio link. This link achieves an impressive data throughput of 100 megabits per second, a rate at least 100 times greater than any other currently available wireless BCI. Operating as an 802.11 WiFi device, the relay station effectively bridges the implant to any compatible computer.
BISC is not merely a hardware solution; it incorporates its own specialized instruction set and a comprehensive software environment, effectively functioning as a dedicated computing system for brain interfaces. The high-bandwidth recording capabilities demonstrated in the study are paramount for enabling advanced machine-learning and deep-learning algorithms to process neural signals. These algorithms can then interpret complex intentions, perceptual experiences, and intricate brain states with unprecedented accuracy. "By integrating everything on one piece of silicon, we’ve shown how brain interfaces can become smaller, safer, and dramatically more powerful," Shepard emphasized.
The advanced semiconductor fabrication techniques employed are foundational to BISC’s capabilities. The implant was manufactured using TSMC’s 0.13-µm Bipolar-CMOS-DMOS (BCD) technology. This sophisticated fabrication method amalgamates three distinct semiconductor technologies onto a single chip, enabling the efficient integration of mixed-signal integrated circuits (ICs). This process allows for the seamless co-existence of digital logic (from CMOS), high-current and high-voltage analog functions (from bipolar and DMOS transistors), and power devices (from DMOS), all of which are critical for BISC’s high-performance operation.
The journey from laboratory innovation to clinical application is a crucial phase for BISC. Shepard’s team has forged a strong partnership with Dr. Youngerman at NewYork-Presbyterian/Columbia University Irving Medical Center to facilitate this transition. They have successfully developed and refined surgical procedures for the safe implantation of the ultra-thin device in preclinical models, confirming its ability to produce high-quality, stable neural recordings. Initial short-term intraoperative studies in human patients are already underway, marking a significant milestone in the clinical validation process.
"These initial studies give us invaluable data about how the device performs in a real surgical setting," Dr. Youngerman stated. He elaborated on the surgical advantages: "The implants can be inserted through a minimally invasive incision in the skull and slid directly onto the surface of the brain in the subdural space. The paper-thin form factor and lack of brain-penetrating electrodes or wires tethering the implant to the skull minimize tissue reactivity and signal degradation over time." This minimally invasive approach significantly reduces the risks associated with traditional brain implants and promises improved long-term performance.
Extensive preclinical work in the motor and visual cortices was conducted in collaboration with Dr. Tolias and Bijan Pesaran, a professor of neurosurgery at the University of Pennsylvania, both distinguished leaders in computational and systems neuroscience. Their contributions were vital in understanding and validating the neural decoding and stimulation capabilities of BISC. "The extreme miniaturization by BISC is very exciting as a platform for new generations of implantable technologies that also interface with the brain with other modalities such as light and sound," remarked Pesaran, underscoring the broader implications of BISC’s miniaturization for future neurotechnology.
The development of BISC was made possible through the Neural Engineering System Design program of the Defense Advanced Research Projects Agency (DARPA). It also benefits from Columbia University’s deep-seated expertise in microelectronics, the advanced neuroscience programs at Stanford and Penn, and the surgical prowess of NewYork-Presbyterian/Columbia University Irving Medical Center. This synergistic collaboration has been instrumental in bringing this complex technology to fruition.
To accelerate the transition of BISC from research to practical clinical use, researchers at Columbia and Stanford have established Kampto Neurotech. This startup, founded by Dr. Nanyu Zeng, an alumnus of Columbia’s electrical engineering program and a lead engineer on the project, is actively producing research-ready versions of the chip and diligently seeking funding to prepare the system for human patient trials. "This is a fundamentally different way of building BCI devices," Zeng asserted. "In this way, BISC has technological capabilities that exceed those of competing devices by many orders of magnitude." This bold claim reflects the significant performance leap BISC represents.
As artificial intelligence continues its rapid advancement, BCIs are increasingly recognized not only for their potential to restore lost functions in individuals with neurological disorders but also for their future role in enhancing normal human capabilities through direct brain-to-computer communication. The convergence of AI and BCI technology is poised to redefine human interaction with machines and unlock new frontiers in human augmentation.
"By combining ultra-high resolution neural recording with fully wireless operation, and pairing that with advanced decoding and stimulation algorithms, we are moving toward a future where the brain and AI systems can interact seamlessly — not just for research, but for human benefit," concluded Shepard. "This could change how we treat brain disorders, how we interface with machines, and ultimately how humans engage with AI." The implications of BISC extend far beyond medical applications, hinting at a future where the boundaries between human cognition and artificial intelligence become increasingly blurred, offering profound benefits for humanity.