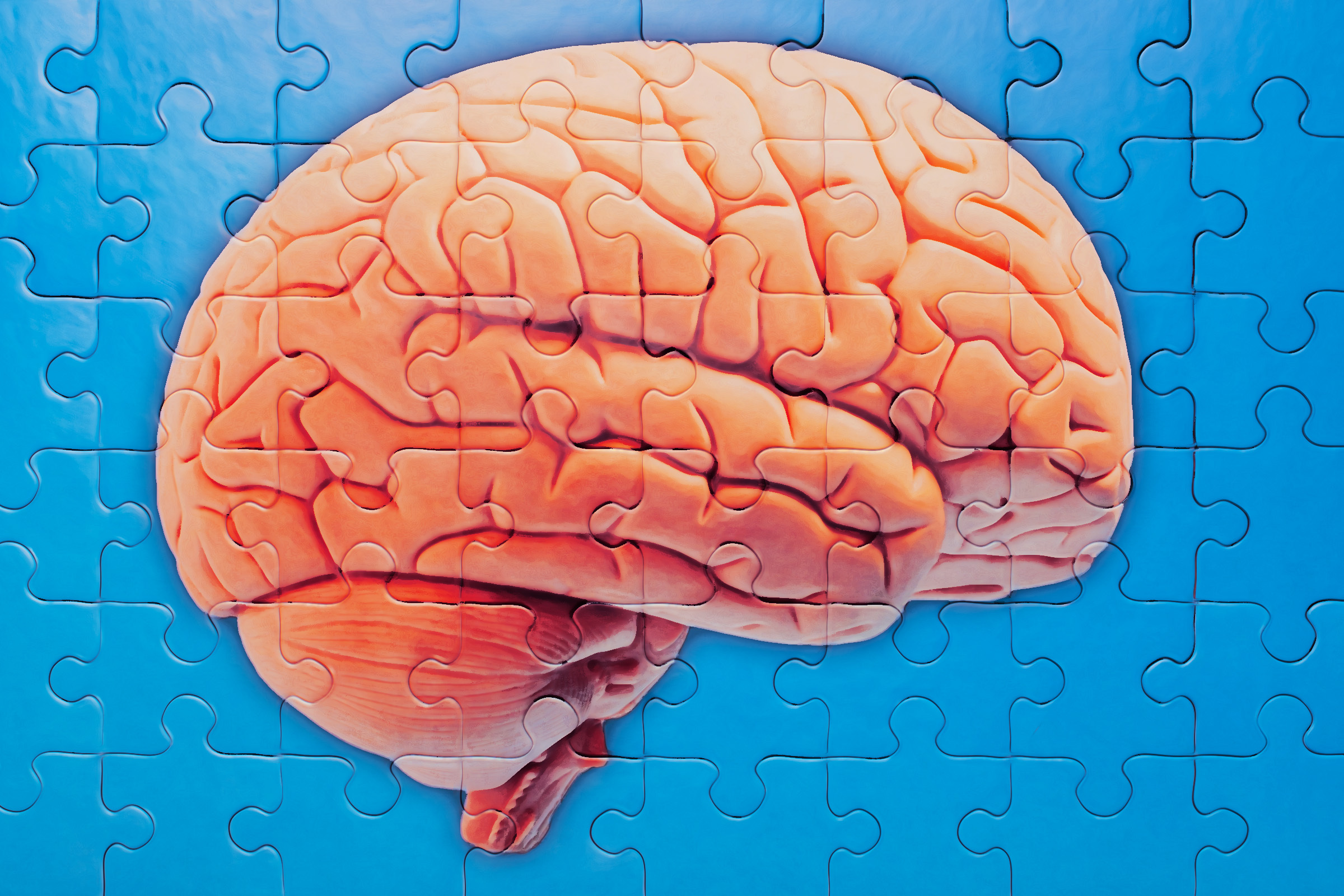
Alzheimer’s disease, a progressive disorder that causes brain cells to degenerate and die, is the most common cause of dementia, characterized by a continuous decline in thinking, behavioral, and social skills that disrupts a person’s ability to function independently. Affecting millions globally, with numbers projected to soar in coming decades, AD currently lacks a cure, and existing treatments primarily focus on managing symptoms rather than arresting or reversing the disease’s progression. This grim reality underscores the monumental significance of any research offering a glimmer of hope, particularly one suggesting a preventative or early-stage intervention.
The team at Northwestern University, renowned for its cutting-edge scientific endeavors, published their groundbreaking findings in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. Their investigation centered on understanding the complex molecular mechanisms underlying AD and identifying new therapeutic targets. A key discovery involved an previously unknown subtype of a brain protein that appears to be a crucial precursor to the disease. This specific protein, now identified, became the primary target for their innovative compound, NU-9.
Richard Silverman, a distinguished chemistry professor at Northwestern and a co-author of the paper, is also the inventor of NU-9, a synthetic compound with the technical designation of cyclohexane-1,3-dione. Silverman articulated the vision for NU-9 by drawing a powerful analogy: "Most people are used to monitoring their cholesterol levels. If you have high cholesterol, it doesn’t mean that you will have a heart attack soon. But it’s time to take drugs to lower your cholesterol levels to prevent that heart attack from happening down the road. NU-9 could play a similar role. If someone has a biomarker signaling Alzheimer’s disease, then they could start taking NU-9 before symptoms appear.” This analogy brilliantly encapsulates the paradigm shift the researchers envision – moving from reactive symptom management to proactive, preventative control.
To test NU-9’s efficacy, the researchers conducted a meticulously designed experiment using laboratory mice genetically predisposed to develop Alzheimer’s disease. Crucially, these mice had not yet exhibited any symptoms of the condition, allowing the team to assess NU-9’s potential as an early intervention. For 60 days, these mice received daily oral doses of NU-9. The scientists paid particular attention to the impact of NU-9 on amyloid beta oligomers (AβOs), which are small, soluble aggregates of amyloid-beta protein. These AβOs are widely considered to be highly neurotoxic and play a critical role in the initiation and progression of Alzheimer’s pathology, accumulating in the brain years before clinical symptoms manifest.
Upon detailed examination of the mice brains after the 60-day treatment period, the findings were nothing short of remarkable. NU-9 significantly decreased the presence of a specific, previously unknown subtype of amyloid beta oligomers, which the researchers dubbed ACU193+ AβOs. This precise identification of a novel, toxic AβO subtype is a critical advancement in itself, as it provides a more refined understanding of the disease’s molecular underpinnings and a more targeted therapeutic opportunity. The team established a clear association between this ACU193+ AβO subtype and brain inflammation, a destructive process known to occur early in the disease progression, often preceding cognitive decline. By introducing NU-9 into these mice brains, the compound effectively tamed the presence of this specific toxic protein and, consequently, dramatically reduced the associated inflammation.
William Klein, a Northwestern neuroscience professor and the principal investigator of the paper, expressed the profound impact of these results, stating, "These results are stunning." He further elaborated on the broader implications: "There are a couple early diagnostic blood tests for Alzheimer’s disease in development. The promise of better early diagnostics — combined with a drug that could stop the disease in its tracks — is the goal." This statement highlights the synergistic potential of emerging diagnostic tools with therapies like NU-9. The ability to identify individuals at high risk for AD before irreversible brain damage occurs, and then intervene with a preventative medication, represents a monumental leap forward in the fight against this disease.
The next logical and crucial step in the research trajectory is to investigate the effectiveness of NU-9 in later stages of Alzheimer’s disease. While early intervention is highly desirable, understanding its potential to slow or reverse progression in individuals already experiencing symptoms is equally vital. Following successful preclinical trials, the path forward would involve rigorous human clinical trials, typically progressing through several phases (Phase 1 for safety, Phase 2 for efficacy and dose-finding, and Phase 3 for large-scale confirmation) to ensure both the safety and effectiveness of NU-9 in human subjects. This process is often lengthy, complex, and resource-intensive, but it is the indispensable bridge between laboratory discovery and patient access.
Richard Silverman’s initial invention of NU-9 was driven by a broader ambition to identify chemical compounds capable of tackling a range of neurological diseases. Indeed, NU-9’s potential extends beyond Alzheimer’s. The compound has also shown promising efficacy against Amyotrophic Lateral Sclerosis (ALS), often referred to as Lou Gehrig’s disease, and potentially against frontotemporal degeneration (FTD). This versatility is not coincidental; all three conditions – Alzheimer’s, ALS, and FTD – share a common pathological thread: the abnormal aggregation of toxic proteins in the brain. In ALS, this often involves proteins like TDP-43, while in FTD, tau or TDP-43 can accumulate. The fact that NU-9 demonstrates efficacy across these distinct but mechanistically similar neurodegenerative diseases suggests it targets a fundamental pathway common to protein misfolding disorders, making it a potentially broad-spectrum therapeutic agent for a range of currently untreatable conditions.
The recognition of NU-9’s profound potential is further underscored by significant institutional backing. The National Institute on Aging (NIA), a primary federal agency for Alzheimer’s research and a component of the National Institutes of Health (NIH), has invested substantial funding, including an additional $7.3 million, into NU-9 research. This level of investment from a leading national health organization signals strong confidence in the compound’s promise and its potential to address an immense unmet medical need.
While the "stunning" results in mice offer a powerful beacon of hope, it is essential to approach these findings with the balanced perspective characteristic of scientific research. The transition from animal models to human therapies, known as translational medicine, is notoriously challenging. Many compounds that show immense promise in preclinical studies fail in human trials due to issues of toxicity, lack of efficacy, or differences in biological systems. However, the specificity of NU-9 in targeting a newly identified, toxic AβO subtype, coupled with its oral bioavailability and potential multi-disease utility, positions it as a particularly exciting candidate. The prospect of an oral medication that could prevent or significantly delay the onset of Alzheimer’s disease, akin to managing high cholesterol, represents a monumental shift in how humanity might confront one of its most feared and debilitating diseases. It offers a tangible vision of a future where Alzheimer’s is no longer an inevitable sentence but a manageable health challenge.