In a groundbreaking announcement that offers a potent beacon of hope in the fight against one of humanity’s most devastating diseases, a collaborative team of American scientists has achieved what many previously considered an impossibility: they have successfully “cured” laboratory mice suffering from Alzheimer’s disease. This remarkable feat, detailed in a new paper published in the esteemed journal Cell Reports Medicine, addresses a condition that has inexorably robbed millions globally – including over seven million Americans, predominantly those aged 65 and above – of their identity, memories, and fundamental cognitive abilities, inflicting immeasurable suffering on patients and their families alike.
The researchers, hailing from Ohio’s Case Western Reserve University (CWRU), University Hospitals, and the Louis Stokes Cleveland VA Medical Center, accomplished this monumental reversal by administering a powerful and unique compound known as P7C3-A20 to the afflicted rodents. Their findings suggest that the insidious effects of Alzheimer’s disease may not be an irreversible destiny, but rather a condition from which the brain, under the right conditions, possesses the capacity to repair itself and regain lost function. This revelation fundamentally shifts the paradigm from merely slowing or preventing the disease to actively reversing its advanced stages.
Andrew A. Pieper, the study’s principal investigator and a distinguished neuroscience professor at CWRU, encapsulated the profound implications of their work in a statement about the research. “The key takeaway is a message of hope – the effects of Alzheimer’s disease may not be inevitably permanent,” Pieper stated. “The damaged brain can, under some conditions, repair itself and regain function.” This statement underscores a significant departure from previous research that largely focused on halting disease progression, offering instead the tantalizing prospect of full neurological recovery.
This study represents a crucial advancement within a burgeoning wave of highly promising laboratory investigations globally, all pointing towards a future where Alzheimer’s disease and other debilitating neurological disorders could become ailments of the past. Beyond this specific P7C3-A20 research, other scientific endeavors have yielded remarkable results in animal models using diverse compounds and innovative treatments, from antibody-based therapies targeting amyloid plaques to novel approaches leveraging gene editing and inflammation modulation. The collective progress is igniting unprecedented excitement among scientists, prompting bold predictions about the imminent arrival of truly transformative treatments.
One such prediction comes from University of Edinburgh neuroscience professor Tara Spires-Jones, who, while not directly involved in the P7C3-A20 study, recently shared her optimistic outlook with the BBC. She believes scientists are closer than ever to a “truly life-changing” treatment, potentially within the next five to ten years. Professor Spires-Jones envisions a future where, instead of a slow and agonizing decline into cognitive oblivion, new diagnostic tests will detect the condition at its earliest stages, allowing innovative treatments to intervene effectively and enable individuals to “really make your life normal.” This vision speaks to a profound shift from managing decline to restoring a full quality of life.
A significant factor contributing to this newfound optimism is the rapidly expanding understanding of Alzheimer’s etiology. Scientists are progressively unraveling the complex web of factors that spark the disease, which appears to be a multifactorial condition influenced by genetics, environmental exposures, lifestyle choices, and various biological stressors. This deeper comprehension suggests that future patients will likely benefit from a personalized cocktail of anti-Alzheimer’s treatments and drugs, meticulously tailored to their unique genetic predispositions, specific biomarkers, and individual disease progression, moving away from a one-size-fits-all approach.
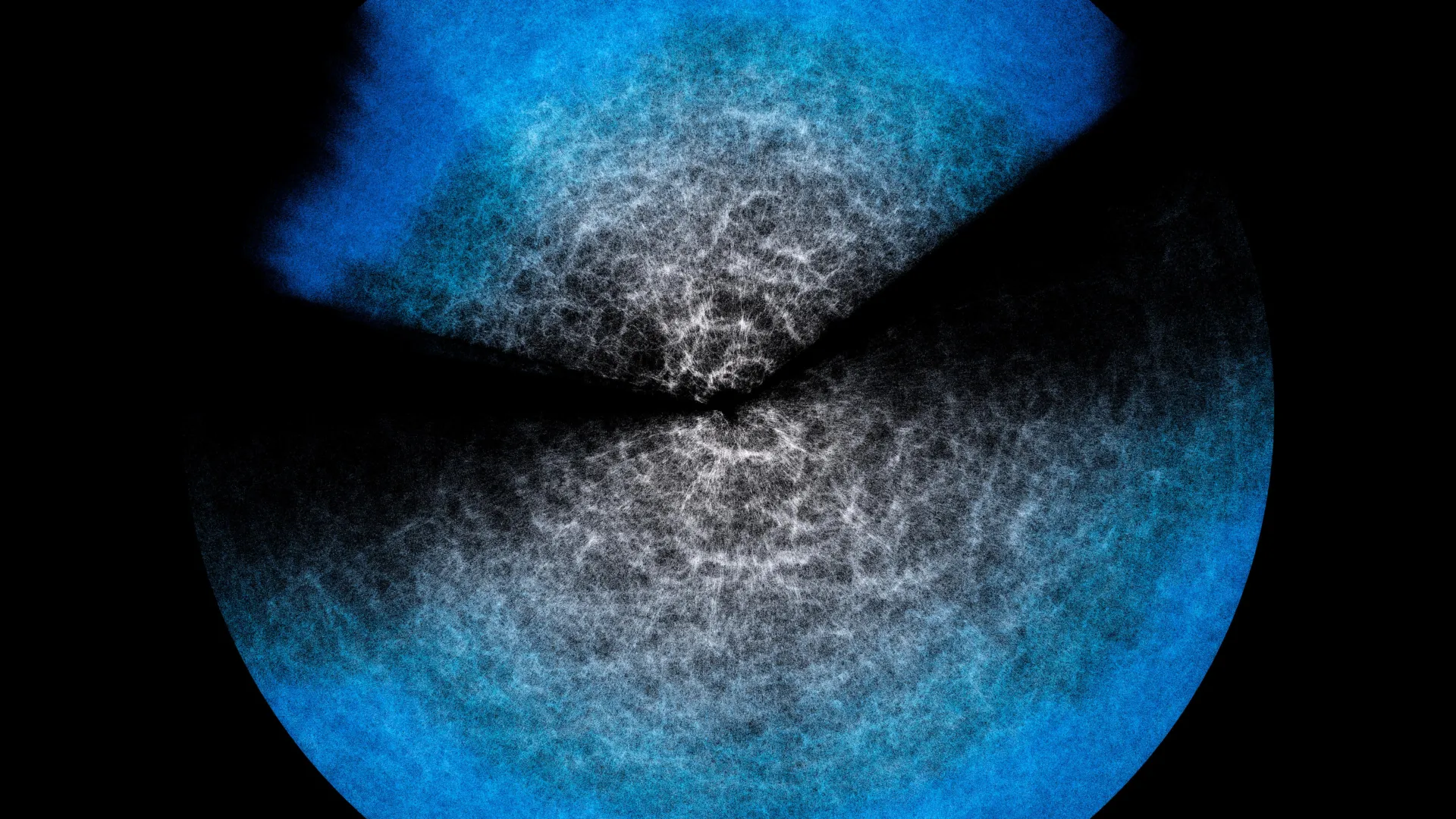
Regardless of the myriad initial causes, previous research has increasingly converged on the idea that Alzheimer’s disease, at its core, involves a significant inflammatory component within the brain. This neuroinflammation is not merely a symptom but a driving force behind neuronal damage and dysfunction. Consequently, a key therapeutic strategy involves not just managing symptoms, but actively lessening or entirely eliminating this chronic inflammation within the brain. This understanding has propelled research into compounds that can modulate the brain’s immune response and restore cellular homeostasis.
The P7C3-A20 study specifically homed in on the critical role of the molecule NAD+ (Nicotinamide Adenine Dinucleotide), a coenzyme that is absolutely essential for driving a vast array of cellular metabolic processes, including energy production, DNA repair, and maintaining mitochondrial function. Critically, NAD+ levels naturally decline as we age, a phenomenon increasingly linked to various age-related diseases. Patients suffering from Alzheimer’s disease exhibit a pronounced decrease of NAD+ in their brains, which directly contributes to their brain cells struggling to maintain normal functionality, effectively stave off inflammation, and counteract the detrimental physical hallmarks of the disease, such as oxidative stress and impaired waste clearance.
To investigate the therapeutic potential of P7C3-A20, the research team utilized two distinct types of lab mice, each genetically engineered to be predisposed to Alzheimer’s. One cohort carried mutations associated with the amyloid precursor protein, leading to the accumulation of amyloid-beta plaques, while the other possessed tau protein mutations, resulting in the formation of neurofibrillary tau tangles. Both amyloid plaques and tau tangles are considered the pathological hallmarks of Alzheimer’s disease. While these proteins are vital for normal cellular function, their aberrant accumulation disrupts synaptic communication, impairs neuronal transport, and ultimately leads to widespread brain cell death.
In the first phase of the study, the team administered P7C3-A20 to both mouse cohorts starting at two months of age, a point before the onset of significant pathology. The results were compelling: this prophylactic treatment successfully prevented the mice from developing the disease altogether, highlighting its potential as a preventative agent. However, the truly monumental discovery emerged from the second phase. Here, a separate batch of lab mice, already suffering from a relatively advanced stage of Alzheimer’s at six months of age – a point analogous to significant cognitive decline in humans – received injections of the compound. The outcome was nothing short of astonishing: these mice not only halted their decline but completely recovered their cognitive ability, and their NAD+ levels were robustly restored to homeostatic, healthy levels. This demonstrated a complete reversal of established disease, a feat rarely observed in Alzheimer’s research.
Pieper expressed the team’s profound excitement regarding these results. “We were very excited and encouraged by our results,” he affirmed. “Restoring the brain’s energy balance achieved pathological and functional recovery in both lines of mice with advanced Alzheimer’s. Seeing this effect in two very different animal models, each driven by different genetic causes, strengthens the new idea that recovery from advanced disease might be possible in people with AD when the brain’s NAD+ balance is restored.” This dual-model success is particularly important as it suggests the therapeutic mechanism targets a fundamental underlying pathology, rather than a specific genetic mutation.
An additional significant advantage of P7C3-A20 is its unique mechanism for boosting NAD+ levels. Unlike many over-the-counter chemical precursors for NAD+, which can elevate NAD+ to potentially toxic levels and have been linked to an increased risk of developing certain cancers, P7C3-A20 offers a safer, more controlled pathway. Pieper cautioned against the widespread availability and unregulated use of these direct NAD+ supplements, which are readily accessible online with just a few clicks. This concern underscores the importance of developing compounds like P7C3-A20 that can safely modulate crucial biological pathways without adverse side effects, prioritizing patient safety in the pursuit of effective treatments.
With such promising preclinical results, the research team is now actively planning to move towards human clinical trials, a critical and rigorous next step in validating these findings in people. However, the compelling nature of the discovery has clearly outpaced the traditional scientific development pipeline for some. A quick online search for P7C3-A20 reveals numerous websites already selling vials of the compound, highlighting a concerning trend of individuals seeking unproven treatments outside of regulated medical channels. This underscores the urgent need for robust clinical trials to determine the safety, efficacy, and appropriate dosage of P7C3-A20 in humans, while also educating the public about the inherent risks of self-medication with unverified substances.
The journey from laboratory discovery to an approved therapeutic is long and arduous, typically spanning years of meticulous testing and regulatory review. Yet, the profound implications of this research – the demonstrated ability to reverse advanced Alzheimer’s pathology and restore cognitive function in animal models – injects an unprecedented level of optimism into the global effort to conquer this devastating disease. It paints a vivid picture of a future where Alzheimer’s is not an inevitable decline, but a manageable or even curable condition, restoring hope and dignity to millions of lives.